This is a rush transcript. Copy may not be in its final form.
AMY GOODMAN: This is Democracy Now!, democracynow.org. I’m Amy Goodman, with Nermeen Shaikh.
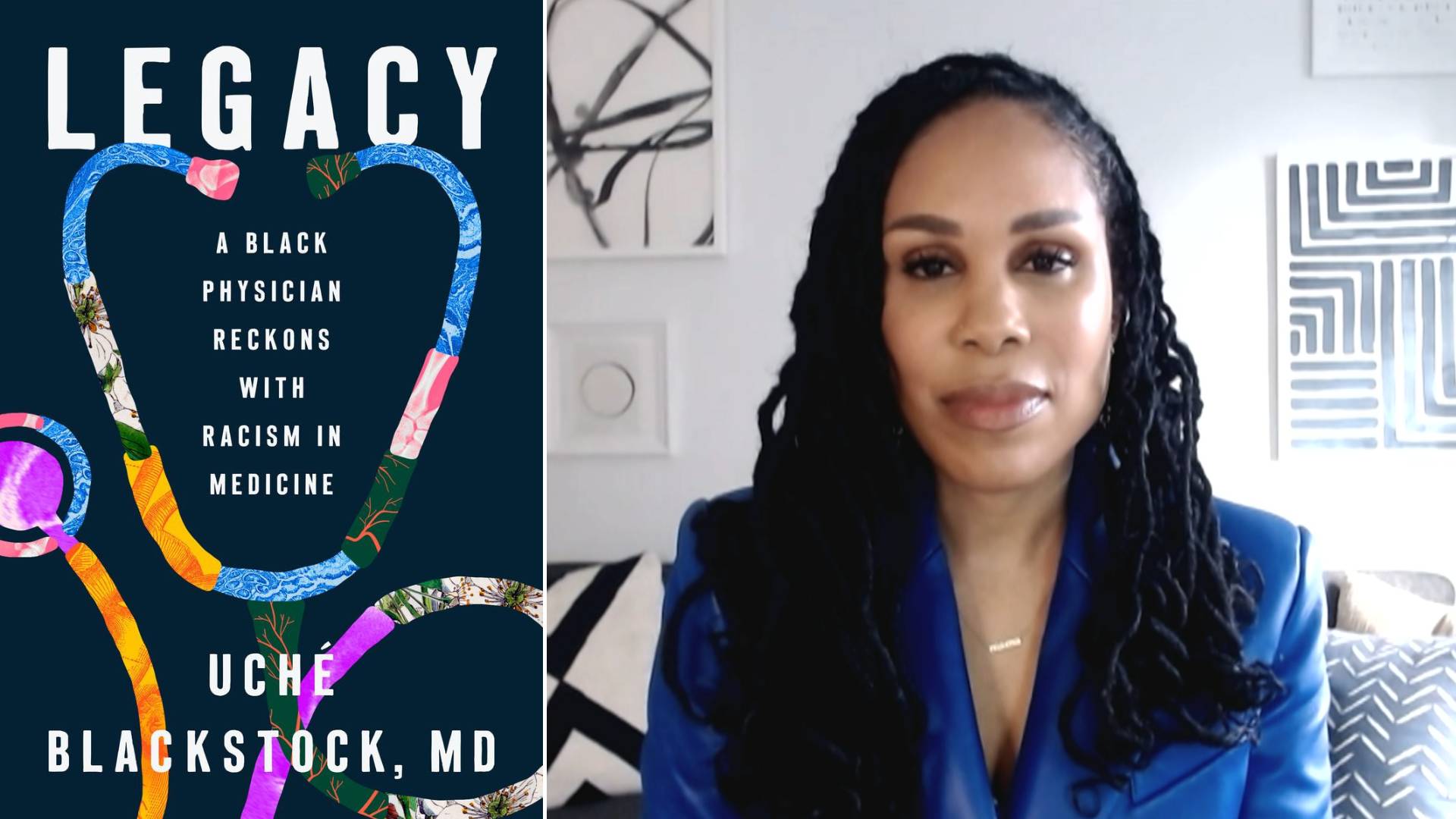
NERMEEN SHAIKH: Today, on the first day of Black History Month, we take a look at how racism shapes healthcare in America. A new book by Dr. Uché Blackstock explores systemic inequity in healthcare throughout the history of the United States up to today, as well as her own family history.
AMY GOODMAN: The book is titled Legacy: A Black Physician Reckons with Racism in Medicine. Dr. Uché Blackstock is an emergency medicine physician, CEO and founder of Advancing Health Equity, a company that works with healthcare organizations to fight racism and bias in services. She joins us today in New York.
Dr. Blackstock, we spoke to you during the pandemic. We’re speaking to you again today. The issue of health equity, or I should say inequity, is pervasive throughout the healthcare system in this country. If you can lay it out? But start off by talking about your family, your groundbreaking mother as a Black woman physician, you and your twin sister, the remarkable work that you’ve done, and why you’re so motivated to take this issue on.
DR. UCHÉ BLACKSTOCK: Well, thank you so much for having me.
You know, I really wanted to write this book as a way to helping readers connect the dots about why, in 2024, we have the worst racial health inequities, despite advances in innovation, research and technology. So I used my own personal story, you know, being a second-generation Black woman physician, which is something that, unfortunately, is still quite rare. My mother was the original Dr. Blackstock, graduated from Harvard Medical School in 1976, but was the first person in her family to go to college, and then medical school, and then came back and returned to Brooklyn, New York, where she grew up, to care for her neighbors and family, and practicing what’s now known as health equity, organizing community health fairs, connecting residents to the social services that they needed, and working with other Black physicians and Black women physicians to do this work in service to their community. And so, I use my mother’s story and my story to really emphasize that — how deeply embedded systemic racism is in our country, in the past and in the present, and to explain why even myself, as a Black woman with a college and medical degree from Harvard, I still am five times more likely to die of pregnancy-related complications than my white peers.
So I wanted use the history to explain why there are so few Black physicians today, and that’s because of a report called the Flexner Report, that we can talk a little bit more about. But I also wanted to explain how there are deeply rooted myths about Black people in this country, essentially biological essentialism, saying that we are different from other people, even though we know race is a social construct. It really is racism through practices and policies that have harmed Black people in this country over the last centuries and have caused us to live shortened lives.
NERMEEN SHAIKH: Dr. Blackstock, you mentioned the Abraham Flexner report, and you said it’s very important. Could you explain what it is and what impact it had on African Americans in medical schools in the early 20th century?
DR. UCHÉ BLACKSTOCK: So, absolutely. I thought it was very important for people to understand one of the reasons why there are so few Black physicians in the United States. You know, we’re over 13% of the U.S. population, but we represent less than 6% of all physicians. And a lot of that has to do with this groundbreaking and actually very harmful report that came out in 1910 that was commissioned by the American Medical Association, which is the oldest and largest organization of physicians and has its own troubling history with bias and racism. American Medical Association and the Carnegie Foundation commissioned Abraham Flexner, who was an education specialist, and also an avid racist — you can tell from his readings that I’ve included in the book. He believed Black people did not deserve to go to medical school, and if they were in medical school, they were there to help their white peers from getting sick.
But anyway, he essentially assessed all 155 medical schools in the United States and Canada and held them up to the criteria of the gold standard, Johns Hopkins at the time. And schools that didn’t meet that standard were recommended to be closed. And as we know, because of the legacy of racism and slavery, historically Black medical schools did not have the resources or the wealth or the endowments to really live up to those standards. So this report in 1910 led to the closure of five out of seven of the historically Black medical schools, which up to that point had trained about 1,500 students.
But a report a few years ago actually estimated if those five medical schools had remained open, they would have trained between 25,000 and 35,000 Black physicians. And we know most likely they would have been Black physicians, because Howard and Meharry, which are the medical schools that remained open, to this day they still train the most Black physicians out of any medical school in the country. But when we think about that number, 25,000 and 35,000 Black physicians, it’s a tremendous loss for our communities, if you can think of all of the hundreds of thousands or millions of patients, Black patients, that could have been cared for, the number of Black students and trainees who could have been mentored, and the research in Black health that could have been done. So, this report in 1910 has had a tremendous and profound ripple effect on the worsening of health outcomes in our communities.
AMY GOODMAN: I wanted to ask you, Dr. Blackstock, about the horror of the remarkable four Black women sprinters in the Rio de Janeiro Olympics in 2016. Years later, three of the women faced life-threatening pregnancy complications. One of them, Tori Bowie, died as a result of those complications. Two others, after she died, Tianna Madison and Allyson Felix, spoke out about their life-threatening situation. You have the cover story of Vanity Fair, Serena Williams talking about what happened in terms of her life-threatening preeclampsia with pregnancy. Beyoncé. They have made this famous, but it means so many other Black women. Why this disproportionate — I think of Erica Garner, in our studio so many times —
DR. UCHÉ BLACKSTOCK: Yes, yes.
AMY GOODMAN: — the remarkable young activist, daughter of Eric Garner, who was killed by police. She dies after her second child is born, at 27.
DR. UCHÉ BLACKSTOCK: Yes, yes. And so, you know, what is really, I think, very important for people to understand, and what I wanted to do with this book, is to really emphasize that, you know, there is nothing biologically wrong with Black people, there’s nothing inherently wrong with us, but there is something very wrong with the social institutions, not just healthcare, within our country that are deeply embedded with bias and racism, so to the point where often when we, Black patients, interface with the healthcare system and health professionals, often our concerns are dismissed, ignored and minimized, even if we are, like Serena Williams, the greatest — one of the greatest athletes of all time. She talks about being ignored by her medical team even after she had a history of a blood clot, telling them she was having similar symptoms. And her symptoms progressed. She almost died.
But also, I want to also point out that for Black people in this country, like, socioeconomic status, educational level of attainment, profession, is not fully protected for us like it is for white people, because racism still causes what The Public Health Researcher terms “weathering.” It still causes a chronic wear and tear on our bodies that causes us to prematurely age and makes us more susceptible to illness and disease.
And so, what I want people to understand, when we see disease and illness in our communities, we see these racial health inequities, they actually are due to a result of upstream factors, like the fact that we live in a capitalist society, the fact that we live in a society where people don’t have healthcare, universal healthcare, the fact that we live in a society with systemic racism, and that illness and disease that we see in Black communities and other communities of color, but specifically in Black communities, is a result of those upstream factors.
So, one thing I do with this book is I want to recommend to health professionals, academic medical institutions, policymakers to think about health in all policies. So, what’s important is that, you know, not just that health professionals are able to adequately and competently care for Black patients and listen to them and give them equitable care, but also that we understand how housing, how education, how employment, how access to quality healthcare, that also impacts how healthy our Black communities are.
NERMEEN SHAIKH: And so, Dr. Blackstock, if you could talk a little bit about your own experience as a healthcare professional and the fact, of course, what you just said, the U.S. has among the worst, if not in the industrialized world the worst, maternal mortality rate? If you could just say, before we end — and we’ll continue in the second part our conversation with you — your own experience working as a doctor?
DR. UCHÉ BLACKSTOCK: Yes. Yes. You know, my own experience — you know, part of this book is also writing about my experience as a physician and being in environments where I, myself, you know, as a Black person, as a Black woman in academic medicine, I felt very silenced. I felt muzzled. I was often questioned by my white patients about, you know, where did I go to medical school. You know, I was in environments that were actually quite toxic, racist and sexist. And that is the case for so many of our Black physicians. Like, all we want to do is — most of us want to work in service to our communities. But I had gotten to the point where, you know, I realized it was too toxic, and I actually left academia. I don’t want that to be the case for everyone. I would love for —
AMY GOODMAN: Dr. Uché Blackstock, we’re going to leave it there but put the rest of the interview at democracynow.org. Her new book, Legacy. I’m Amy Goodman, with Nermeen Shaikh.










Post comments (0)